Transplant rejection is a critical challenge in solid organ transplantation, occurring when the recipient’s immune system recognizes the transplanted organ as foreign and mounts an attack against it.
The Open Science Institute’s Organ Transplantation Initiative has now progressed to the third phase — in silico modeling. We need your support to move forward. Our goal is to raise $750,000 to research and reveal to the scientific community, highlighting the powerful potential of green tea in Organ Transplantation. Please support this initiative.
Transplant rejection is a critical challenge in solid organ transplantation, occurring when the recipient’s immune system recognizes the transplanted organ as foreign and mounts an attack against it. This immune response is driven by the recognition of donor antigens by the host’s T cells, triggering the release of pro-inflammatory cytokines and the activation of both innate and adaptive immune responses. Rejection can manifest in different forms—hyperacute, acute, and chronic—each with varying onset and severity. Hyperacute rejection happens within minutes due to pre-existing antibodies, while acute rejection typically occurs days to weeks post-transplant, primarily mediated by T cells and cytotoxic immune responses. Chronic rejection, a long-term complication, involves gradual tissue damage and fibrosis, leading to organ failure over time. Despite advancements in immunosuppressive therapies, rejection remains a significant cause of graft loss and patient morbidity. These drugs, while effective, carry risks of infection and other side effects. Therefore, exploring safer and more targeted immunomodulatory strategies is crucial. Understanding the cellular and molecular mechanisms of rejection can lead to innovative treatments—such as natural compounds like those in green tea—which offer the potential to promote immune tolerance while minimizing adverse effects, ultimately enhancing transplant survival rates.
The Systems Architecture of Organ Transplantation is published as a Web-based tool open to public. Click below to interact with the systems architecture
A peer-reviewed publication from the Organ Transplantation Initiative has been released in the journal of Clinical Nutrition ESPEN—support this initiative to advance scientific discovery and deliver real solutions.
In this phase, the Organ transplantaion Initiative in silico modeling to identify and test the efficacy of bioactive compounds of green tea on immunomodulation of transplant rejection. The results are shown below.
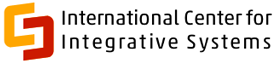
A: Effect of EGCG from green tea on IL-12 induced IFN-γ in naïve T cells. B: Effect of EGCG from green tea on IL-12 induced TNF-α production in naïve T cells.
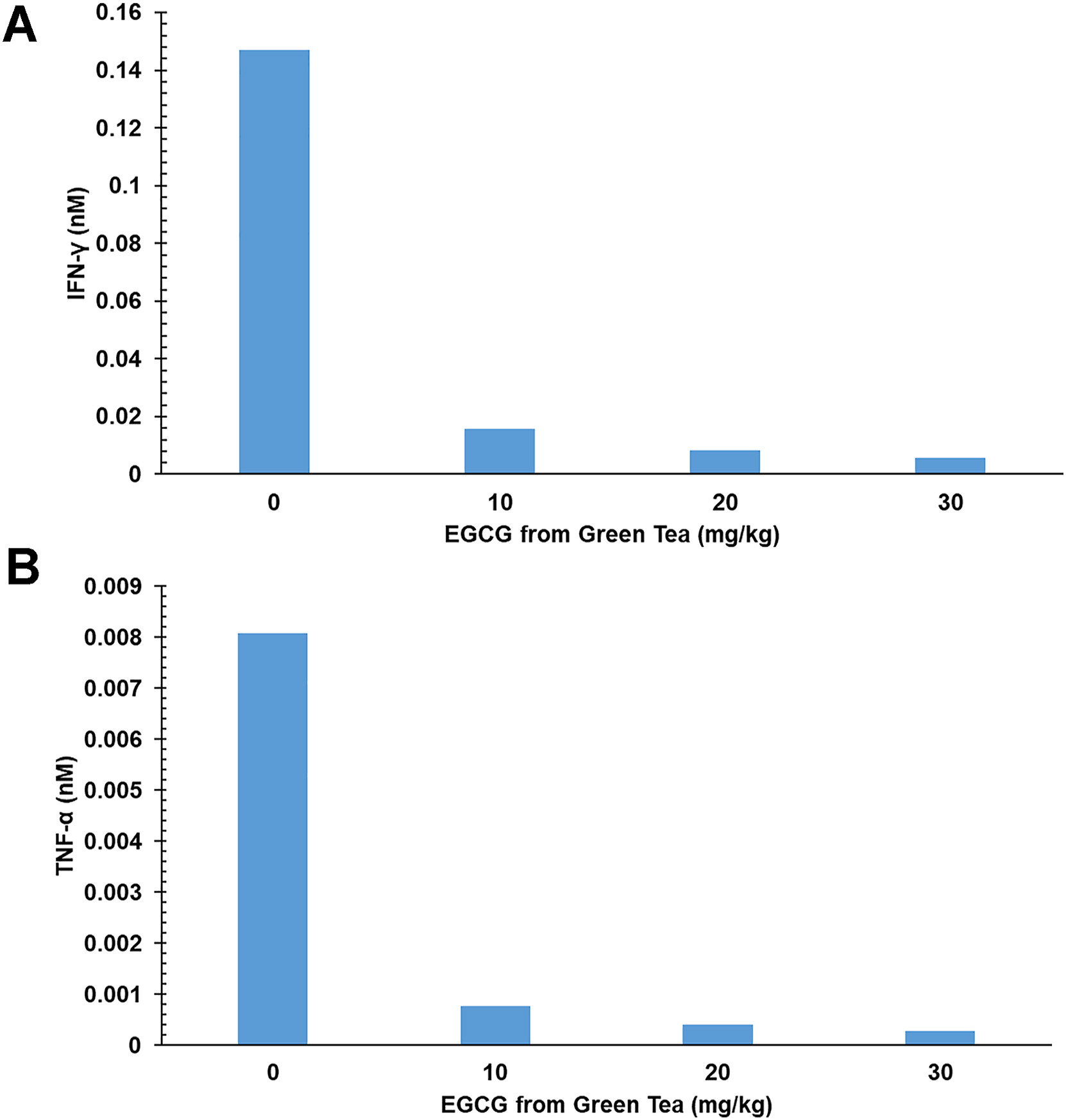
Effect of EGCG from green tea on IL-6 mediated IL-17 production in naïve T cells.
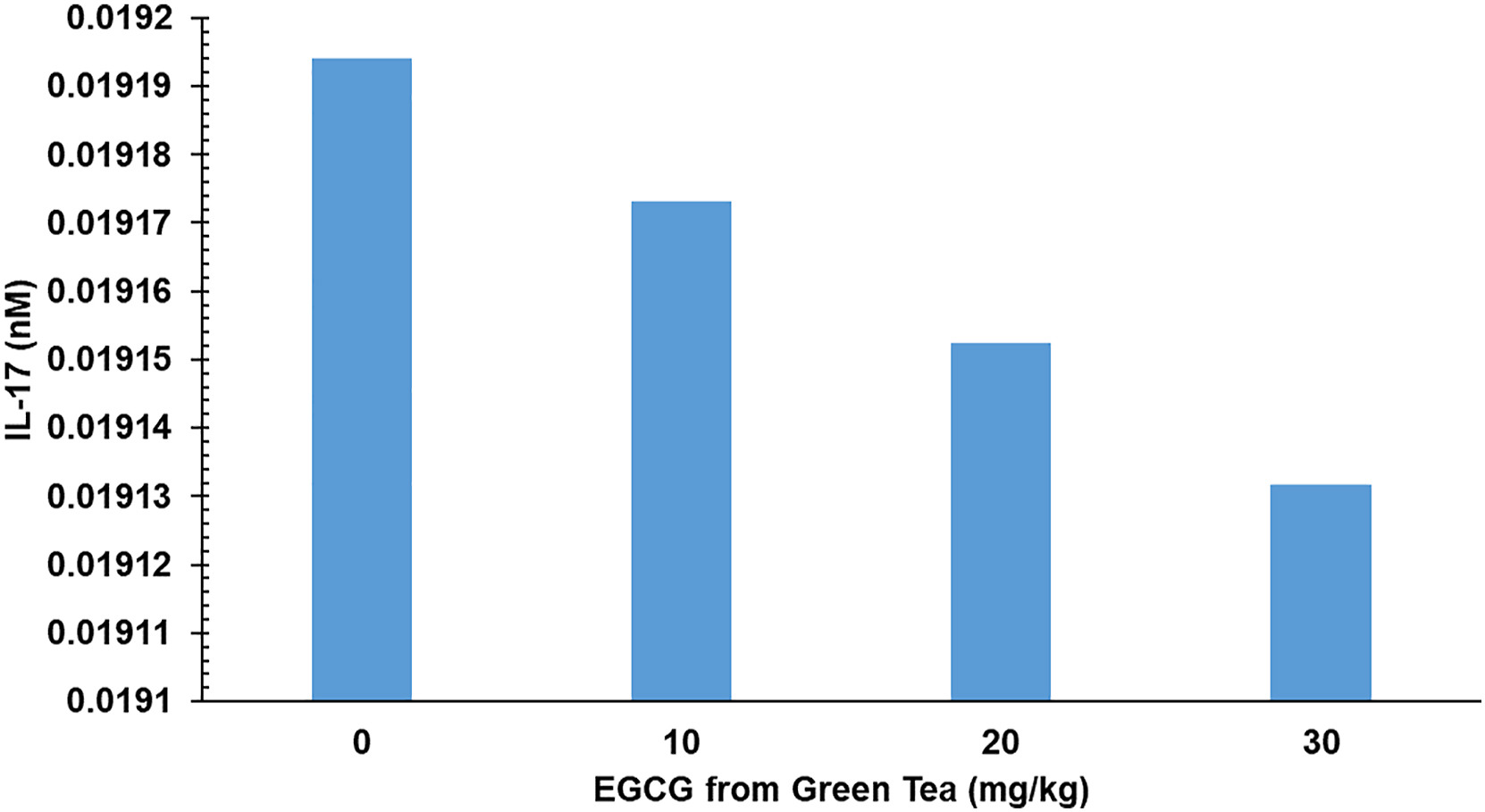
Effect of EGCG on TNF-α mediated Foxp3 production in naïve T cells.
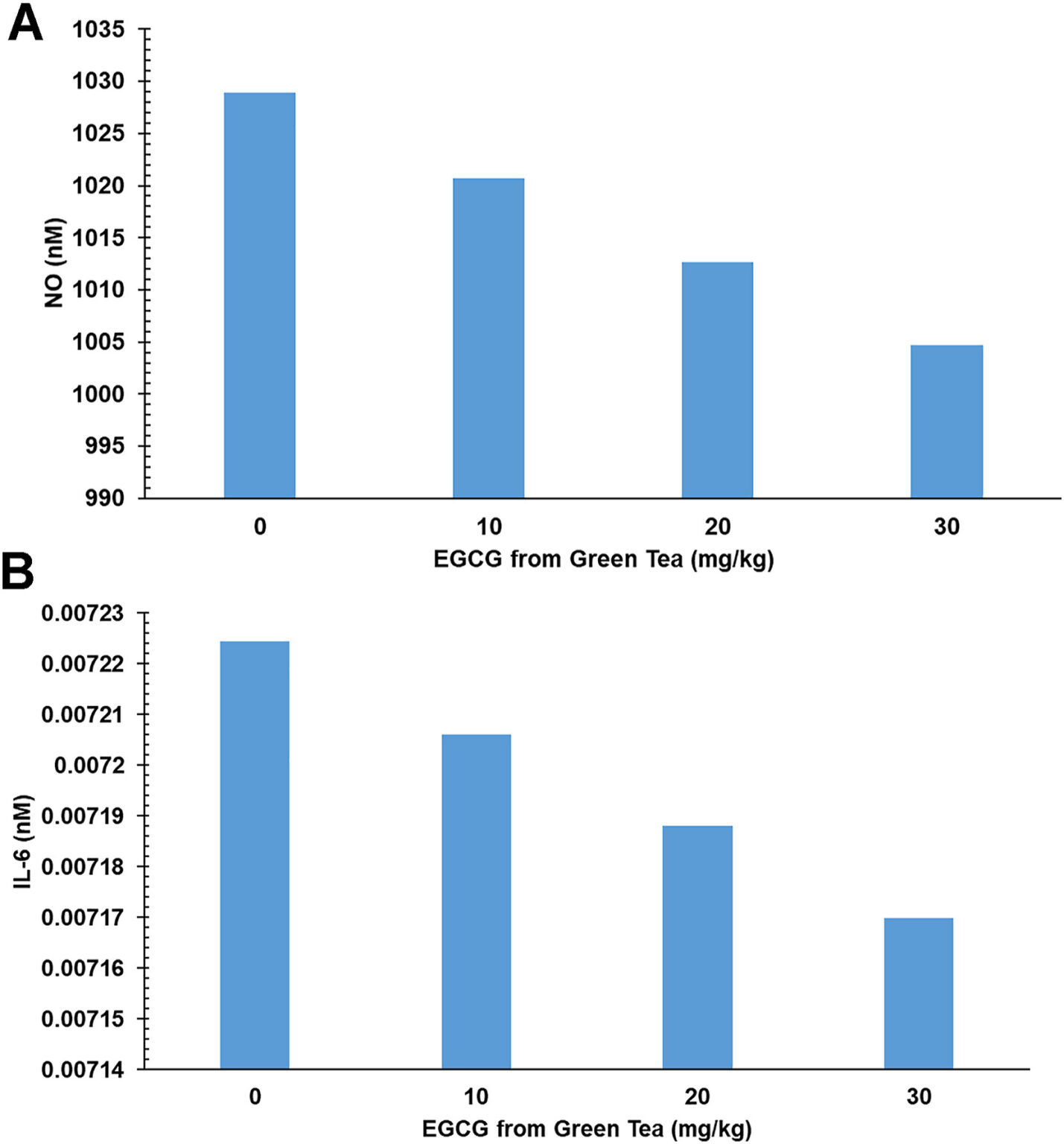
A: Effect of EGCG on TNF-α mediated NO production in naïve T cells. B: Effect of EGCG on TNF-α mediated IL-6 production in naïve T cells.
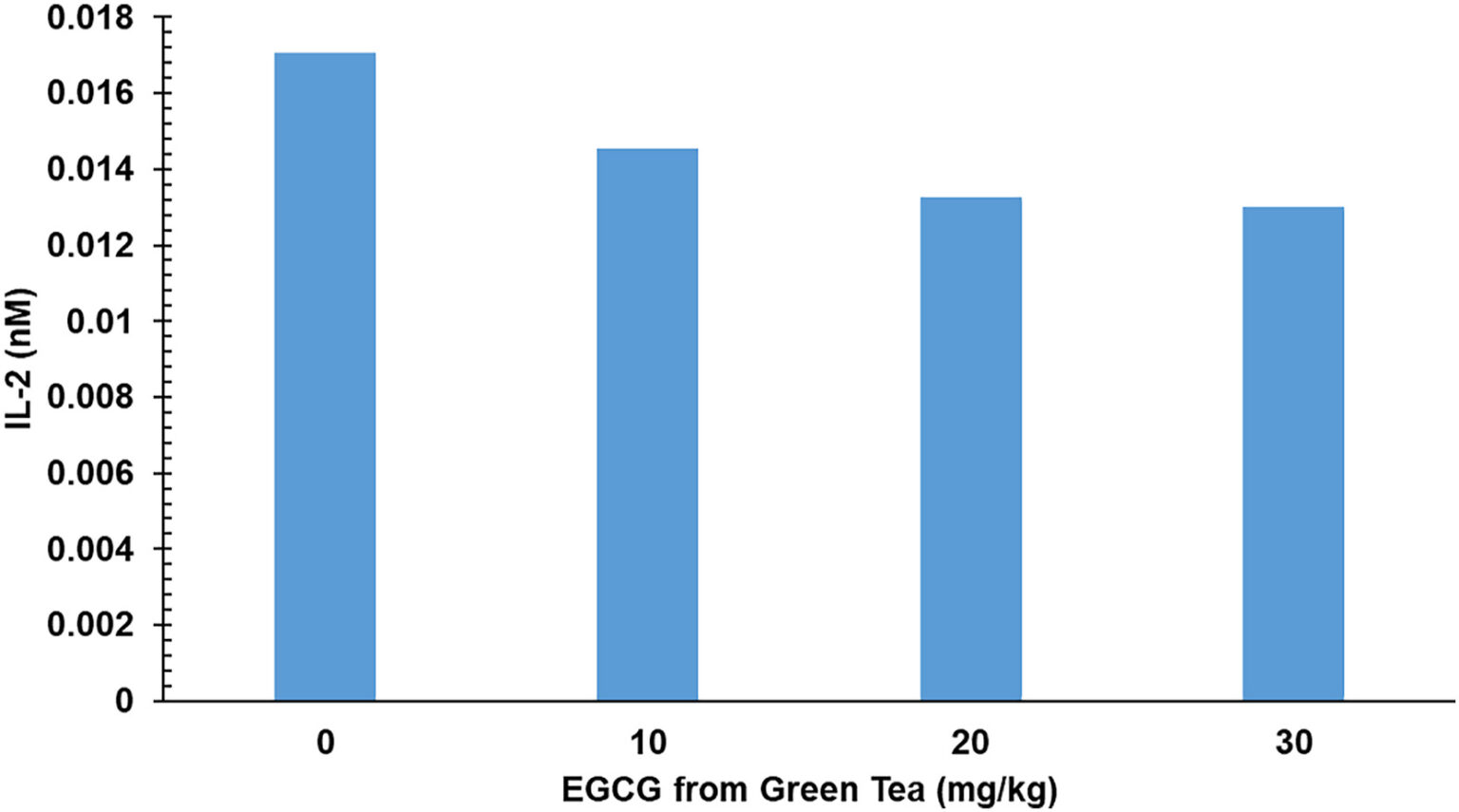
Effect of EGCG on IL-2 in naïve T cells.
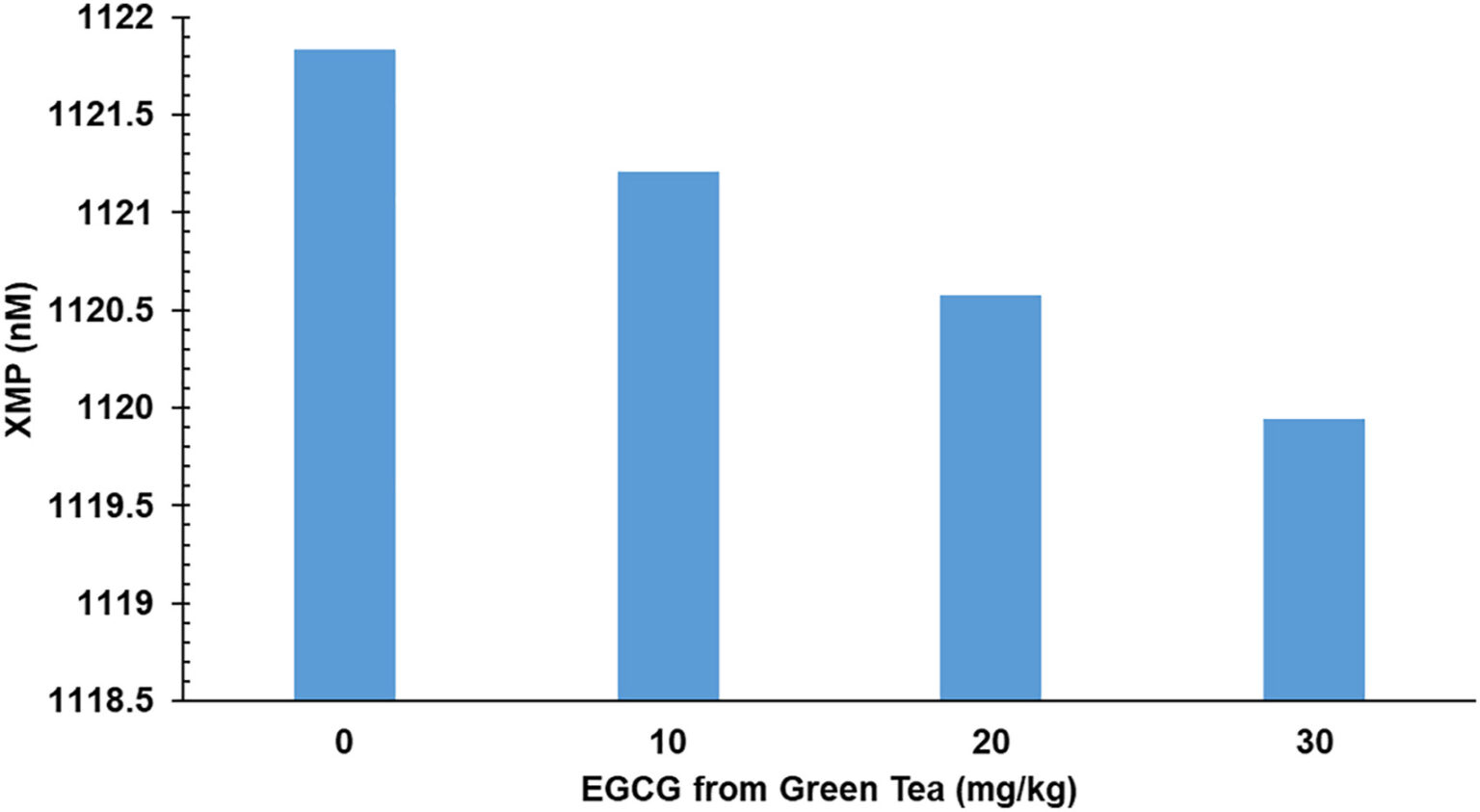
Effect of EGCG on XMP in naïve T cells.
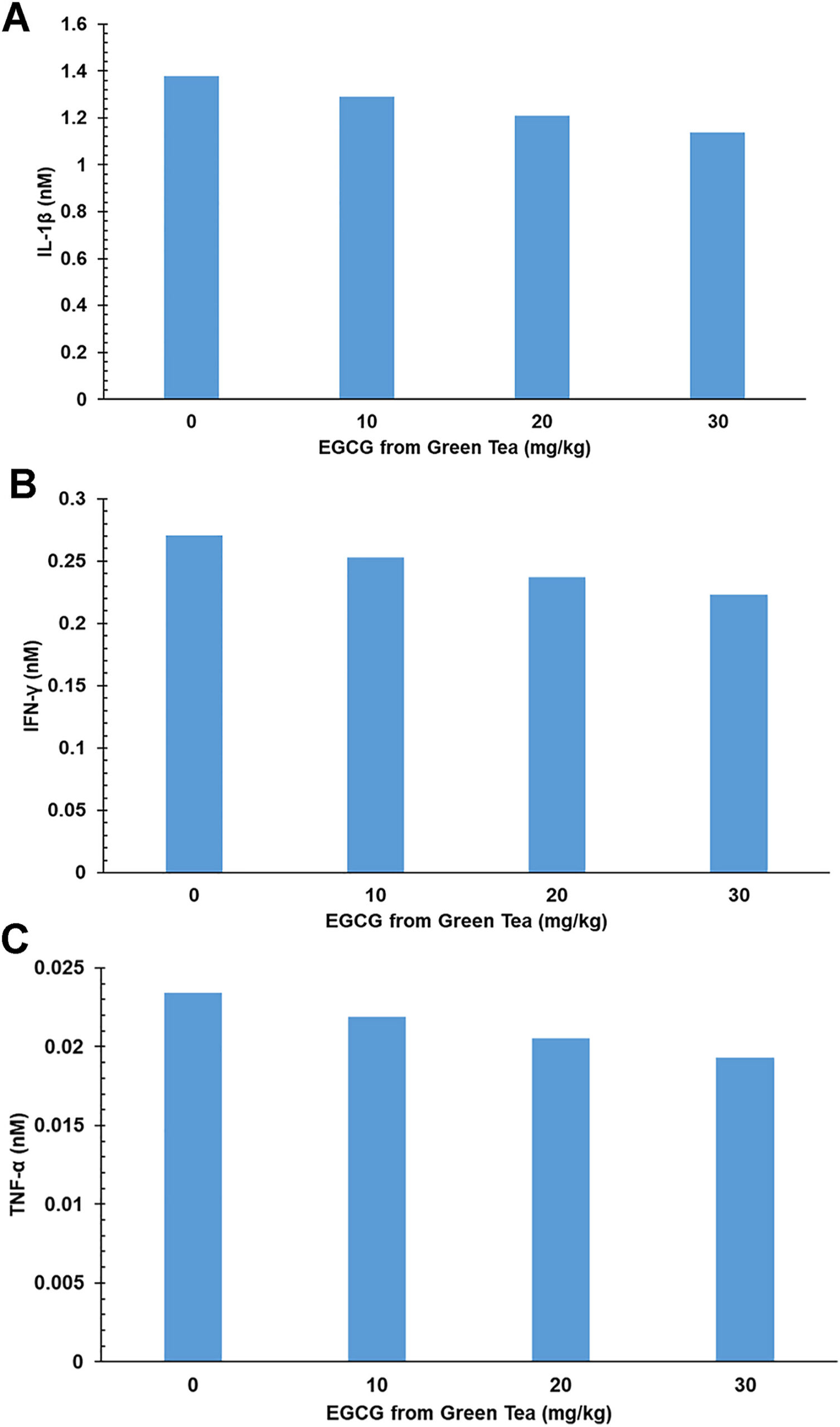
A: Effect of EGCG on IL-1β in dendritic cells. B: Effect of EGCG on IFN-γ in dendritic cells. C: Effect of EGCG on TNF-α in dendritic cells.
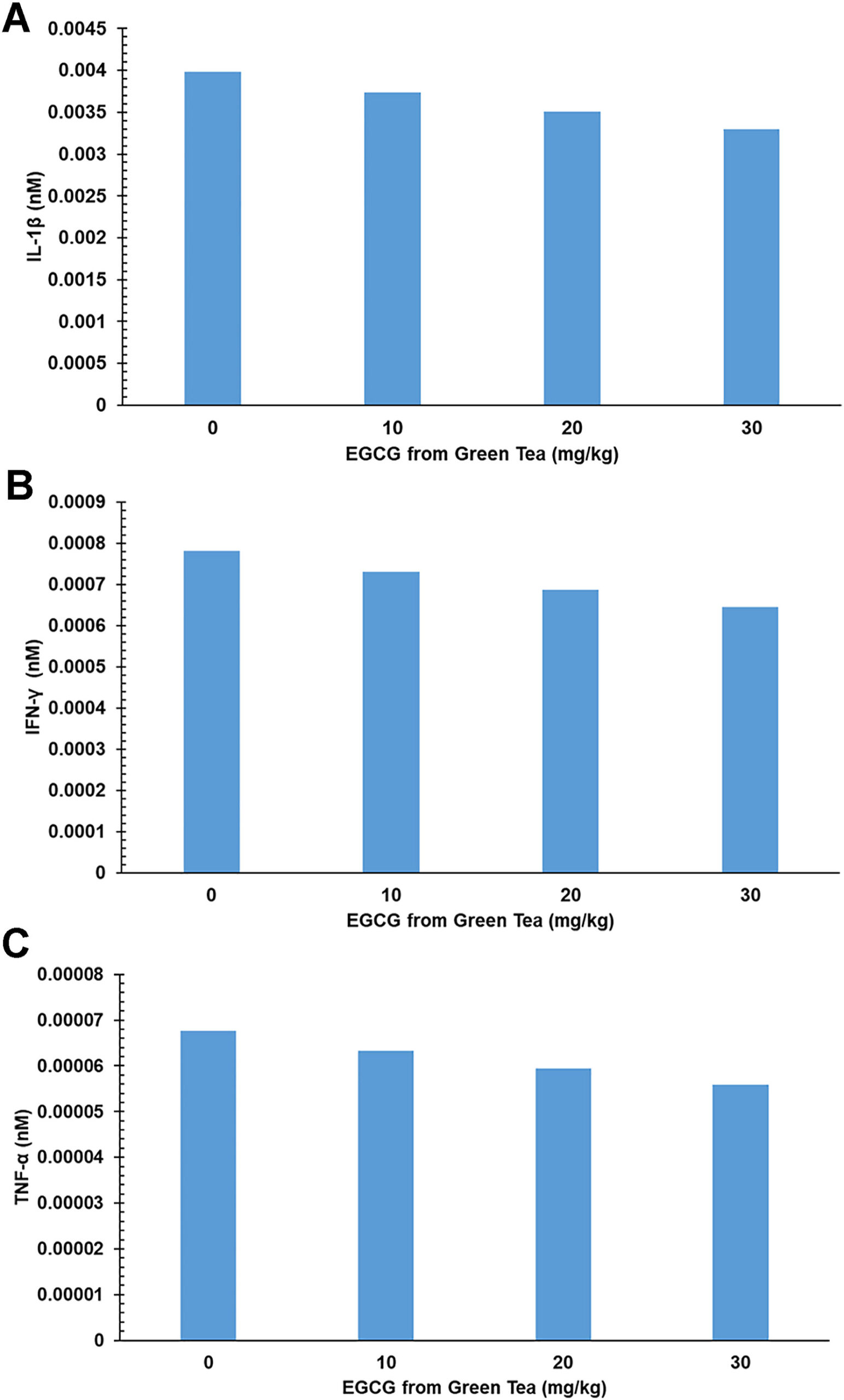
A: Effect of EGCG on IL-1β in dendritic cells. B: Effect of EGCG on IFN-γ in dendritic cells. C: Effect of EGCG on TNF-α in dendritic cells.
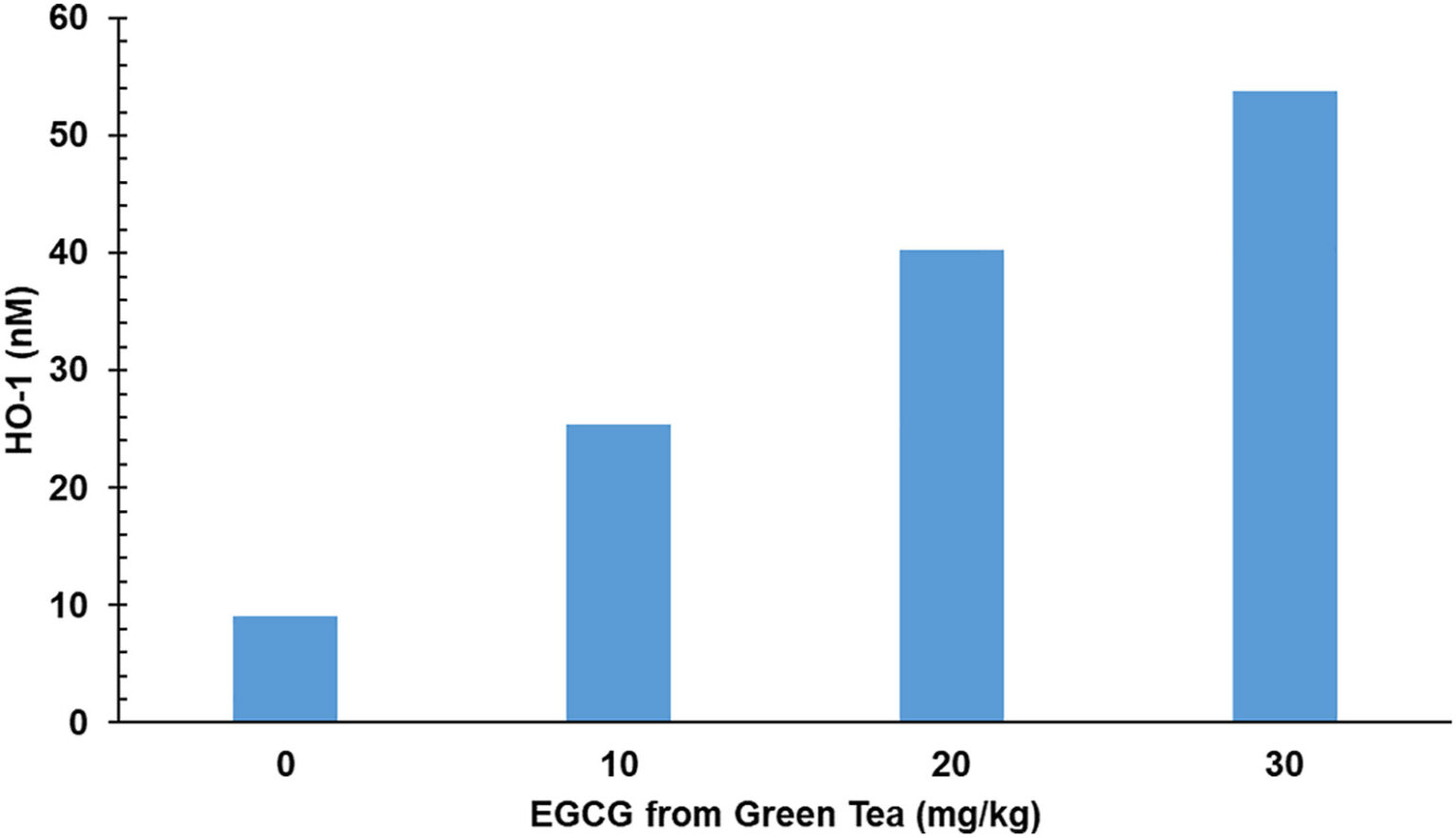
Effect of EGCG on HO-1 in dendritic cell.
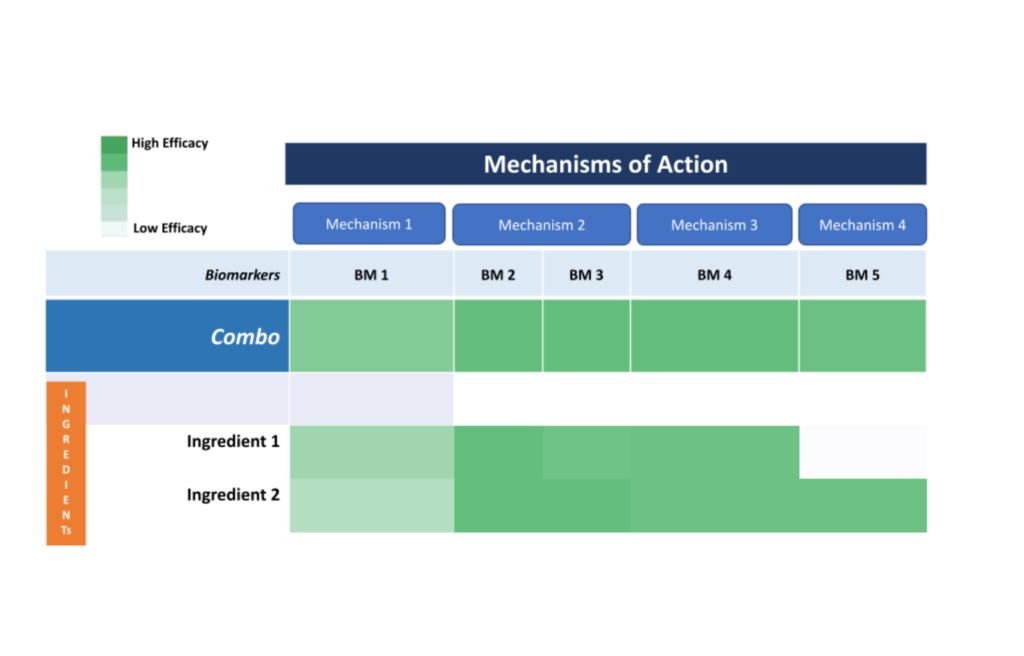
In this phase, combination screening will be performed to identify potential ingredient/compounds that target the biological process implicated in organ transplantation pathogenesis. This phase is in progress.
The Open Science Institute® through its Organ transplantaion initiative is moving towards getting patents for a revolutionary Green tea compounds that affects inflammation, Transplant tolerance and Transplant rejection activity.
The Organ transplantation Initiative plans to discover, develop, license and manufacture a Transplant tolerance product which supports organ transplanted individuals. Support our mission to bring this innovation to those who need it most. Please support this phase by donating to the Organ transplantation Initiative