Lupus Initiative
Lupus, or systemic lupus erythematosus (SLE), is a chronic autoimmune disease in which the body’s immune system mistakenly attacks its own healthy tissues and organs. This can lead to inflammation and damage affecting various parts of the body, including the skin, joints, kidneys, brain, heart, and lungs. Because it can affect so many different systems, lupus is often called “the great imitator.”
The exact cause of lupus is unknown, but it’s believed to involve a combination of genetic, hormonal, and environmental factors. It’s more common in women, particularly during their childbearing years, and certain ethnic groups are also more susceptible.
Lupus is characterized by periods of illness, called flares, where symptoms worsen, alternating with times of remission when symptoms improve or disappear. Symptoms can vary widely from person to person and can change over time. Some common symptoms include extreme fatigue, joint pain and swelling, skin rashes (the butterfly-shaped rash across the cheeks and nose is a classic sign), fever, hair loss, and sensitivity to sunlight.
Diagnosing lupus can be challenging due to its diverse symptoms and the fact that there’s no single definitive test. Doctors typically rely on a combination of medical history, physical examination, blood tests (like the antinuclear antibody or ANA test), and urine tests.
While there’s no cure for lupus, the goal of treatment is to manage symptoms, reduce inflammation, prevent organ damage, and minimize flares. Treatment plans are highly individualized and may involve medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, antimalarial drugs, immunosuppressants, and biologics. With proper management and ongoing medical care, many people with lupus can lead fulfilling lives

Research Progress
.
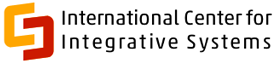
The Open Science Institute’s Lupus Initiative has now progressed to the first phase — Systems architecture.
We need your support to move forward. Our goal is to raise $2 Million to research and reveal to the scientific community, highlighting the powerful potential of herbal ingredients on immune health. Please support this initiative.
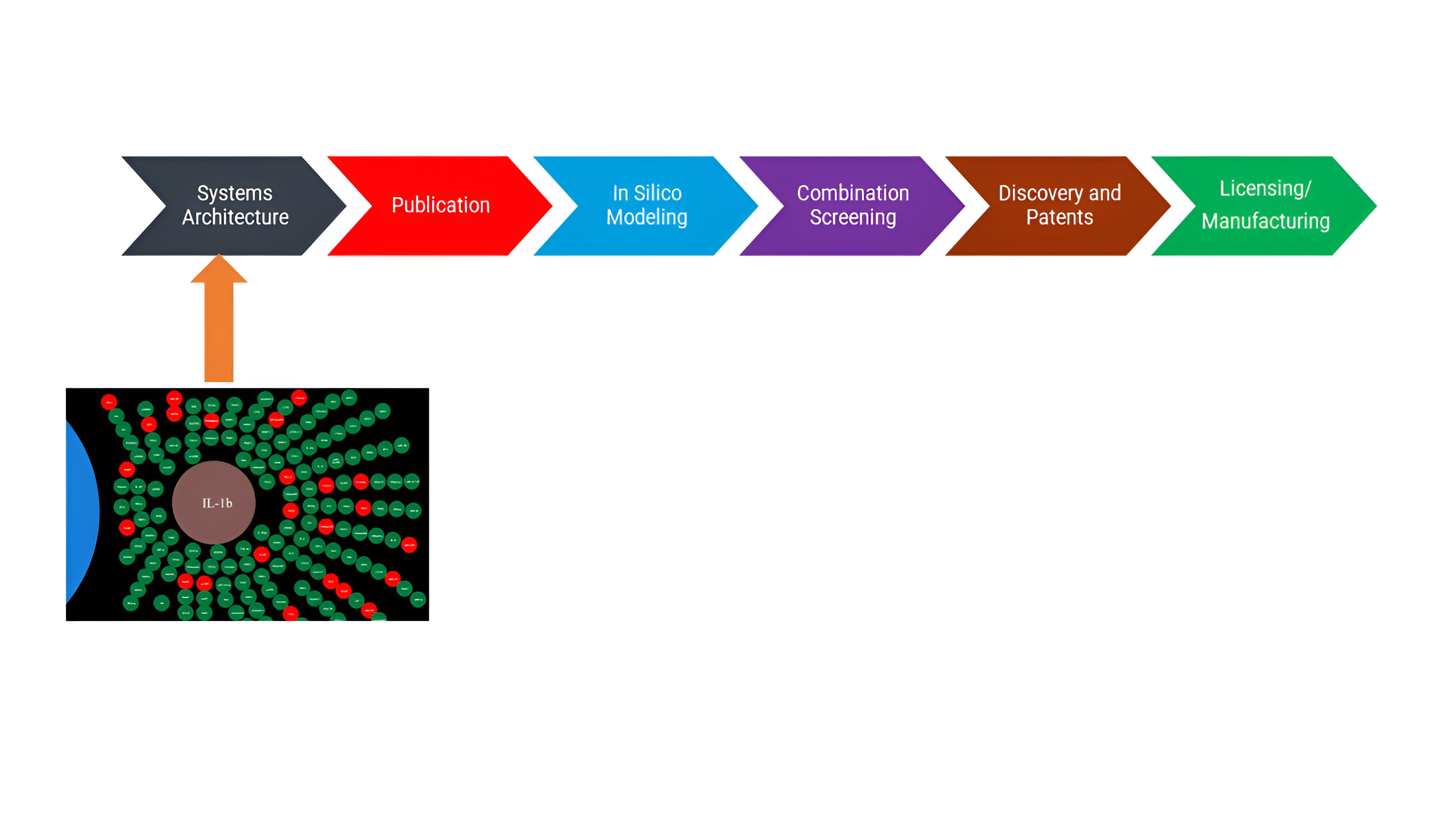
Systems Architecture
The Systems Architecture of Lupus Reseach is published as a Web-based tool open to public. Click below to interact with the systems architecture
Publication
A peer-reviewed publication from the Lupus Initiative will be released soon to benefit the public by revealing powerful insights into the use of herbs for treating Lupus—support this initiative to advance scientific discovery and deliver real solutions.
In silico Modeling
In this phase, the Lupus Initiative will conduct in silico modeling to identify and test the efficacy of compounds on Autoimmunity, Inflammation and Tissue damage activity. This phase is yet to begin.
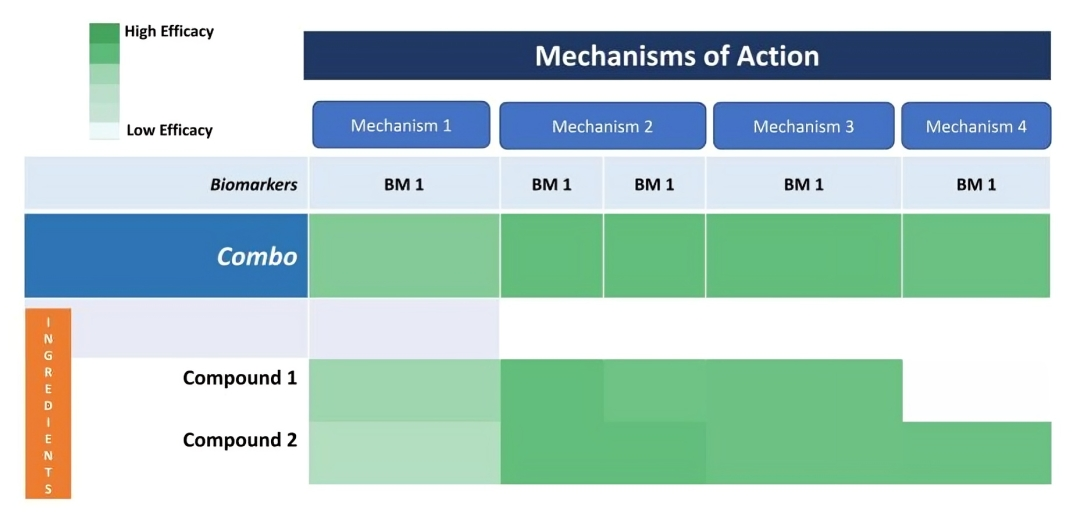
Combination Screening
Patents
The Open Science Institute® through its Lupus initiative is moving towards getting patents for a revolutionary compounds that affects Autoimmunity, Inflammation and Tissue damage activity.
Licensing and Manufacturing
The Lupus Initiative plans to discover, develop, license and manufacture a Lupus product which supports treatment of many diseases. Support our mission to bring this innovation to those who need it most. Please support this Phase by donating to the Lupus Initiative