-Draft-
Version 1.0. Last Updated: June 11, 2025
Web-Enabled Molecular Systems Architecture of Periodontitis
Supplementary Information To
Molecular Systems Architecture of Host-Microbiome Interactions in Periodontitis
V.A. Shiva Ayyadurai1,2, Prabhakar Deonikar1,2 & Philip Stashenko31Systems Biology Group, CytoSolve Research Division, CytoSolve, Inc., Cambridge, MA2Open Science Institute, International Center for Integrative Systems, Cambridge, MA3Departments of Translational Dental Medicine and Departmetn of Endodontics, Goldman School of Dental Medicine, Boston University, Boston, MA
Summary
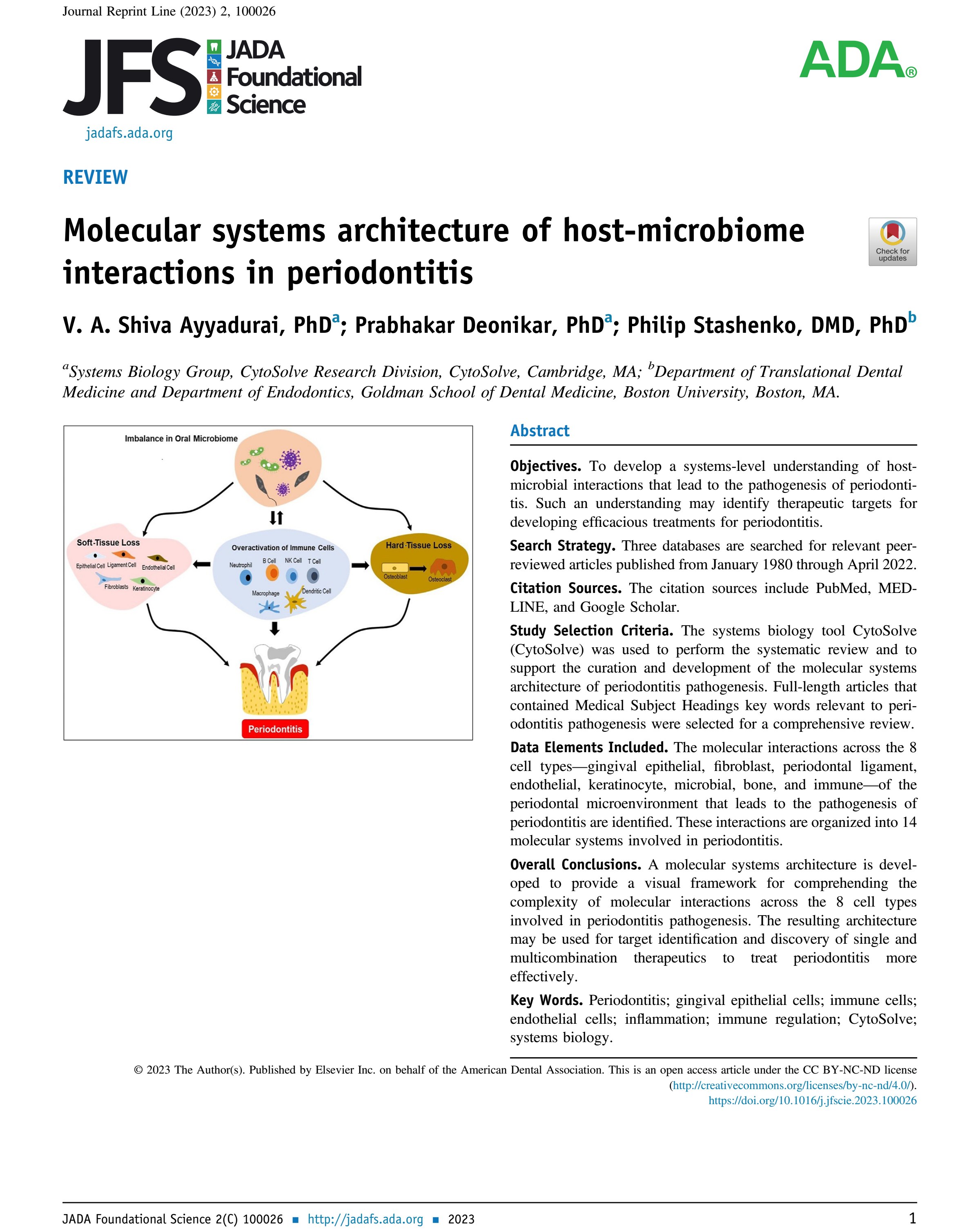
Periodontitis is a complex, multifactorial disease arising from disruptions in host-microbiome homeostasis, leading to inflammation, soft-tissue degradation, and alveolar bone loss. This study employs a systems biology approach using the CytoSolve® computational platform to develop a comprehensive molecular systems architecture that elucidates the interactive signaling pathways among microbial, immune, and host periodontal cell types. A systematic review of literature spanning 1980–2022 curated data on eight key cell types involved in the periodontitis microenvironment: gingival epithelial cells, fibroblasts, periodontal ligament cells, endothelial cells, keratinocytes, immune cells, bone cells, and microbial cells.
The study maps 14 molecular systems implicated in periodontitis, focusing on key pathways such as IL-8, IL-6, TLR4, C5aR, RANKL, and gingipain-mediated signaling. Porphyromonas gingivalis is identified as a keystone pathogen that modulates host signaling to evade immune clearance, inhibit neutrophil function, and enhance osteoclastogenesis via RANKL upregulation. The architecture reveals critical crosstalk that leads to immune dysregulation, soft-tissue loss, and bone resorption.
The resulting three-layered architecture offers a visual and mechanistic framework for understanding disease progression and identifying therapeutic targets. It enables identification of intervention points that may inhibit inflammation, promote tissue preservation, and restore homeostasis. The study sets the stage for future in silico modeling and open-source collaborative research in periodontitis, and proposes this systems architecture as a foundational tool for drug development and personalized therapeutic strategies.
Table of Contents
Original Publication
Epithelial Cell Signaling
IL-4 Signaling
Microbiome Signaling
Osteoblast Signaling
Endothelial Signaling
Th-17 Signaling
Macrophage Signaling
IL-12 Signaling
Feedback
Original Publication